Joint pain(arthralgia) can occur in a single or simultaneously in several joints (polyarthralgia). Arthralgias are observed in rheumatic, endocrine, infectious, tumor, neurological, autoimmune diseases, injuries, overweight. Finding out the causes of joint pain has an important differential diagnostic significance; performed using X-ray, ultrasound, laboratory, invasive methods (arthrocentesis, arthroscopy). Treatment of arthralgia is reduced to the treatment of the disease that caused it. Symptomatic measures are applied (analgesics, local heat, ointments), immobilization, physiotherapy, surgical interventions.
Classification
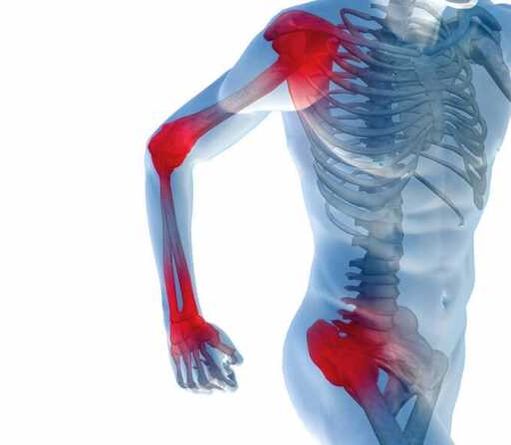
Arthralgias differ in localization and depth, the number of joints involved, the nature and intensity of the pain syndrome, its daily rhythm, duration of existence, connection with a certain type of movement. In the presence of pain in a single joint, they speak of monoarthralgia, with simultaneous or sequential pain syndrome in several joints - about oligoarthralgia, with the involvement of 5 or more joints - about polyarthralgia syndrome.
According to the nature of the arthralgic syndrome, acute and dull pain are distinguished; by intensity - from weak and moderate to intense; according to the type of flow - transient and constant. More often, arthralgia occurs in large joints - the hip, knee, shoulder and elbow, less often in medium and small - wrist, ankle, interphalangeal.
The occurrence of joint pain is promoted by irritation of the neuroreceptors of the synovial membranes of the articular capsules with inflammatory mediators, products of immune reactions, salt crystals, toxins, osteophytes. In rheumatology, it is customary to distinguish the following types of joint pain:
- caused by toxic syndrome in acute infections;
- primary episode or intermittent (intermittent) arthralgia in acute or recurrent arthritis;
- long-term monoarthralgia of large joints;
- oligo- or polyarthralgic syndrome accompanying the involvement of the synovial membranes or progressive degenerative-dystrophic changes in the cartilage;
- residual post-inflammatory or post-traumatic arthralgia in the joints;
- pseudoarthralgia.
Why do joints hurt
Common infectious diseases
Arthralgic syndrome often accompanies the course of acute infections. Joint pain can be observed both in the prodromal period of the disease, and in the early clinical stage, occurring with fever and intoxication. The infectious form of arthralgia is characterized by "ache" in the joints of the lower and upper extremities, the polyarticular nature of pain, and their association with myalgia. The mobility in the joint is completely preserved. Usually, infectious arthralgia disappears within a few days as the toxic syndrome caused by the underlying disease weakens.
Infectious arthritis
Possible options for the development of post-infectious reactive arthralgia after acute intestinal or urogenital infections; parainfectious arthralgic syndrome caused by tuberculosis, infective endocarditis, secondary syphilis. Often the cause of pain in the joints are the foci of the existing chronic infection - pyelonephritis, cholangitis, adnexitis, paratonsillar abscess or parasitic invasion.
Residual arthralgia after inflammation of the joints are chronic or transient. Pain and stiffness in the joints may persist for weeks or months; in the future, the well-being and functions of the limbs are fully restored. In the chronic form of arthralgia, its exacerbations are associated with overstrain, meteorological lability, and hypothermia.

Rheumatic diseases
Joint pain of the type of poly- or ologarthralgia is the main symptom of inflammatory rheumatic diseases. Rheumatic arthralgia is characterized by constant, intense, migrating pain syndrome, involvement of large joints, mainly of the lower extremities, limited movement in the joints.
The debut of rheumatoid arthritis, as well as systemic rheumatic diseases, are manifested by polyarticular syndrome, which affects small symmetrical joints of the feet and hands, motor stiffness in the morning.
In microcrystalline gouty arthritis, arthralgia manifests itself in the form of recurrent paroxysmal pains in an isolated joint, which, having suddenly arisen, quickly reach peak intensity and do not subside for several days.
Degenerative joint lesions
Gradually increasing pain in the joints for a long time may indicate deforming osteoarthritis and other degenerative-dystrophic lesions. In this case, involvement of the knee or hip joints is typical; dull, aching, exercise-related type of pain and their disappearance at rest. Arthralgia can be weather-dependent, accompanied by a "crunching" of the joints during movement, weaken when using local distraction therapy.
Joint injuries
Bruises, dislocations of the joints, damage to the ligamentous apparatus, intra-articular fractures are accompanied by severe pain. The affected joint becomes swollen, deformed, hot to the touch. The support function of the lower limb is impaired, movements in the joint are difficult, and sometimes pathological mobility occurs. Injuries can be accompanied by hemorrhage into the joint cavity, which leads to its stiffness.
Oncological diseases
Persistent oligo- and polyarthralgia of a long course, accompanied by the formation of "Hippocratic fingers" (deformities of the nails and distal phalanges like "watch glass" and "drum sticks"), indicate a paraneoplastic lesion of the synovial membranes. In such patients, oncological pathology of the internal organs, primarily lung cancer, should be suspected.
Endocrine diseases
Common causes of joint pain are endocrine disorders - primary hyperparathyroidism, ovariogenic dysfunctions, hypothyroidism, obesity. Articular syndrome of endocrine genesis proceeds in the form of oligoarthralgia associated with ossalgia, myalgia, pain in the pelvic bones and spine.
Other reasons
Other possible causes of arthralgia include:
- intoxication with heavy metals (thallium, beryllium);
- frequent overload or microtrauma of the joints;
- long-term drug therapy;
- post-allergic reactions;
- flat feet;
- X-shaped or O-shaped deformation of the limbs;
- pseudoarthralgia, simulated by primary ossalgia, neuralgia, myalgia, vascular pathology, psychosomatic disorders.
Diagnostics
Since joint pain is only a subjective symptom, clinical and anamnestic characteristics and physical examination come to the fore when determining the causes of their occurrence. It is necessary to consult a rheumatologist, orthopedist. In order to differentiate the etiology of arthralgia, a number of objective studies are being carried out:
- X-ray of the joints.It is a routine method that allows you to examine any joints in various diseases. Most often, radiography is performed in one or 2 projections, it is also possible to study in special styling, conduct contrast arthrography. A more detailed picture of the state of the osteochondral and soft tissues of the joints is available with CT and MRI imaging.
- Joint ultrasound.Allows you to detect effusion in the joint cavity, bone erosion, changes in the synovial membrane, measure the width of the joint spaces. The availability of sonography makes it indispensable for the diagnosis of rheumatic joint pathologies.
- invasive methods.According to the indications, a puncture of the joint, a biopsy of the synovial membrane is performed. In disputable cases, diagnostic arthroscopy is carried out, which allows to examine the joint cavity from the inside, to carry out diagnostic and therapeutic measures.
- Laboratory tests.Helps to identify the presence of an inflammatory process,rheumatic diseases. In the peripheral blood, the ESR, the level of C-reactive protein, uric acid, specific markers of immunopathology (rheumatoid factor, antinuclear antibodies, ACCP) are determined. An important diagnostic method is the microbiological and cytological examination of the synovial fluid.
- Additional diagnostic methods:thermography, podography.

Treatment
Help before diagnosis
For any pain in the joints, it is necessary to remain calm and not load the limb. Metabolic causes of arthralgia dictate the need for a balanced diet, weight normalization. With fresh injuries, it is necessary to apply cold to the joint, immobilize the injured limb with a splint or fixing bandage. You can take painkillers or NSAIDs.
Neglect of competent examination and treatment for arthralgia is fraught with the development of irreversible functional disorders of the joints - rigidity, ankylosis, contracture. Since pain in the joints can serve as a marker of a wide variety of diseases, it is necessary to consult a doctor if the articular syndrome occurs and persists for more than 2 days.
Conservative therapy
In the treatment of joint pain, the main role is given to the treatment of the leading pathology. Drug treatment of arthralgia is aimed at stopping inflammatory intra-articular processes and pain. Systemic therapy includes the use of non-steroidal anti-inflammatory drugs.
With moderate arthralgia or the presence of contraindications to oral administration of drugs, local external therapy is performed with warming, anti-inflammatory and analgesic ointments. Applications with dimethyl sulfoxide are applied to the joint area. Articular gymnastics, physiotherapy procedures (drug electrophoresis, magnetotherapy, phonophoresis, UHF therapy) are recommended.
If necessary, periarticular blockades, intra-articular injections of glucocorticoids, chondroprotectors, synovial fluid prostheses are performed. Promising modern methods of treatment of chronic articular pathologies are ozone therapy, plasmolifting of joints, orthokine therapy.
Surgery
Various types of surgical interventions are justified for pain in the joints caused by injuries, as well as chronic diseases leading to loss of joint function. They can be performed by open (arthrotomy) or endoscopic (arthroscopy) methods. Depending on the causative disease, the following are performed:
- arthroplasty;
- arthrodesis;
- ligament plastic;
- rehabilitation of the joint cavity;
- removal of pathological formations (cysts, intraarticular bodies);
- synovectomy;
- joint arthroplasty.






















